FROM STABILIZING
TO SUSTAINABILITY
AND SYSTEM BUILDING
CMHO’s 2025 Pre-Budget Submission
Our 2025 Ontario Budget Recommendations
For too many years, we have seen rising prevalence of mental health needs and increasing acuity of mental health issues in children and youth. At the same time, child and youth mental health agencies have faced increasing health human resources challenges that contribute to longer wait times and service gaps. In the 2025 Ontario Budget, we are asking the government to continue partnering with us to invest $42 million in year 1, plus an additional $47 million in year 2, and $53 million in year 3, for a total new annualized investment of $142 million, to help meet current needs and address increasing demands for mental health services.
Our kids and families can’t wait.
Data from the Canadian Institute for Health Information showed that in 2022,
over 27% of hospitalizations
in Ontario for children and youth are due to child and youth mental health issues.
The Case for Continued and Urgently-Needed Investments
Despite investments from the government since 2018, rising demand for services and mental health needs among children and youth combined with workforce shortages mean there is still a significant and urgent need for new investments. Increased and targeted investments in community child and youth mental health will take pressures off other parts of the health care and social services systems and, more importantly, ensure that mental health issues across the continuum of need are addressed timely and equitability.
Rising Prevalence, Demand, and Severity of Child and Youth Mental Health Challenges
Data over the last several years has indicated a greater prevalence of need, increasing acuity (e.g., eating disorders), and differential effects on specific populations, meaning that challenges accessing care and rising demand remain ongoing issues. New investments, while welcome, have not kept pace with demand.
Too many young people and their families are in crisis because they can’t get the help they need, and data from the Canadian Institute for Health Information showed that in 2022, over one in four hospitalizations in Ontario for children and youth are due to child and youth mental health issues. Additional evidence that points to increasing mental health needs and demand for services include:
Of the top 10 reasons children and youth ages 5 to 17 were hospitalized, mental health issues took the first, second, fourth, and tenth spots.
Among these needs, we saw and continue to see significant increases in serious mental health concerns such as eating disorders, self-harm, schizophrenia, and substance use.
Northern regions experienced double the rates of hospital utilization compared to the provincial average.
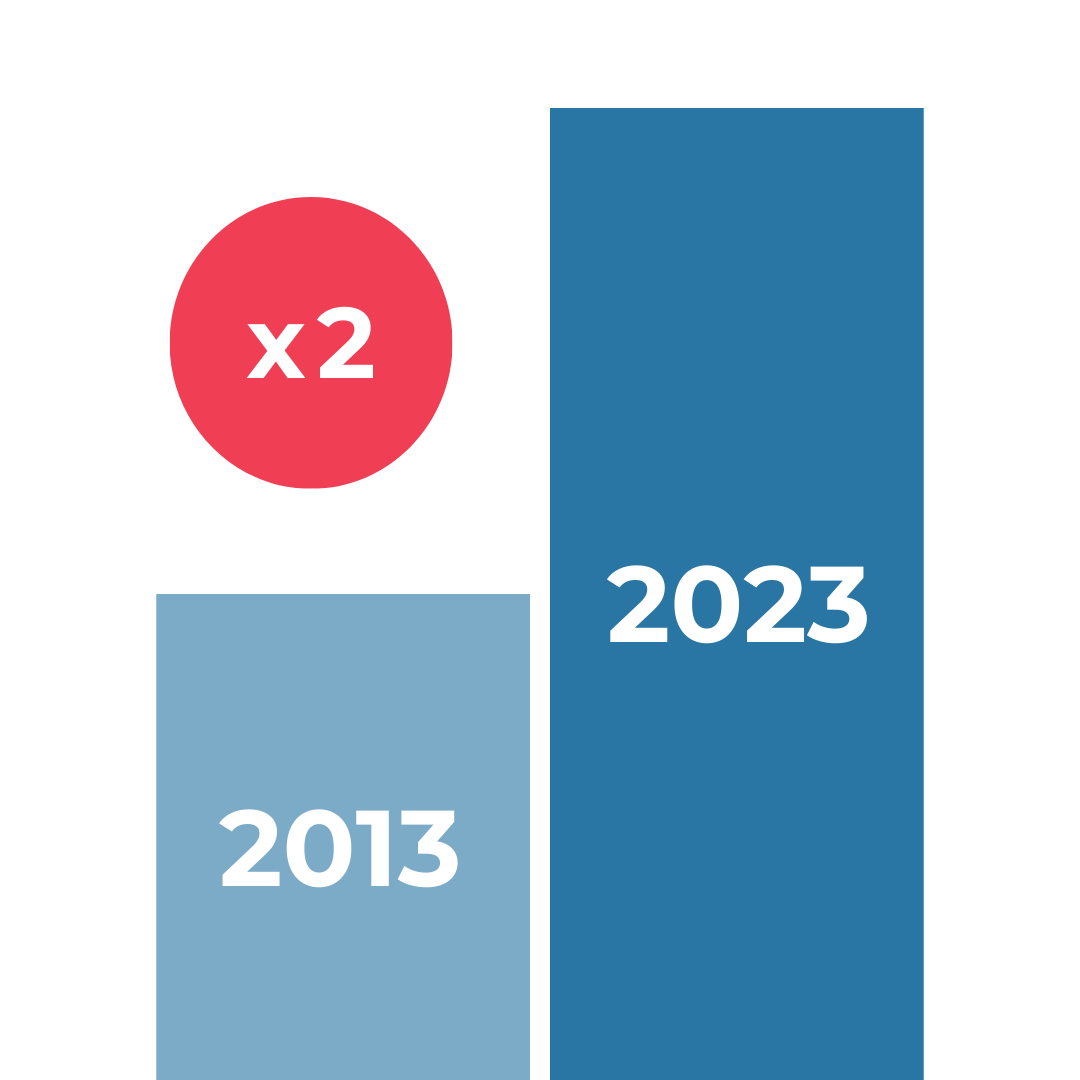
Data from the Ontario Student Drug Use and Health Survey show a significant increase in psychological distress over the last decade with both moderate and serious distress having more than doubled between 2013 and 2023.
Long Wait Times and Service Gaps, Particularly for Equity-Deserving Groups
As a result of the health human resources challenges and rising demand and mental health needs, long wait times and gaps in access to care are the reality for too many Ontario families who require mental health treatment and supports. At last count, there were 28,000 children and youth waiting an average of nine months—some as long as two and a half years—for mental health treatment in Ontario.
These gaps and barriers can be even higher for those with concurrent or co-occurring needs, and those from equity-deserving communities, transition-aged youth, or those from northern, rural and remote communities.
Reduced access to care and mistrust of health care systems for racialized and marginalized populations, as well as a lack of treatment options that are culturally appropriate, identity affirming, and responsive to their experiences and intersecting needs, are gaps that need to be filled in our sector. At the same time, Black, Indigenous, and racialized youth and those navigating their sexual orientation and gender identity have the highest rates of anxiety and depression.
600 days.
That’s how long wait times can be for services in the north.
Health Human Resource Shortages
It is critical to continue to build on previous investments to close the wage gap and develop a workforce strategy. In some agencies, vacancy rates can be as high as 30% and turnover rates as high as 20%. High vacancy and turnover rates of specialized mental health staff contribute to long wait times and families turning to hospitals in crisis, as specialized staff are drawn away from community-based agencies to other sectors like education and hospitals that offer wages that are 20% to 50% higher.
These health human resources challenges have a real and tangible impact on the delivery of care. For children and young people receiving treatment, it is disheartening to have to re-tell your story and potentially lose the progress you were making when your therapist changes and continuity is disrupted. Wait times and wait lists can grow during periods of turnover as new staff have to be recruited, onboarded, and trained before they can carry a full case load.
Moving from Stabilizing to Sustainability
and System Building
The case for continued investments is strong, and the needs of infants, children, youth, and families are urgent. Investments of $42 million in the 2025/2026 budget, plus a multi-year commitment that provides an additional $47 million in year 2 and $53 million in year 3, will enable community child and youth mental health to prioritize stabilizing and move towards sustainability and system building by advancing the following priorities:

STABILIZE
Retaining and recruiting the specialized mental health professionals and inter-professional care teams at community-based child and youth mental health centers is critical to sustaining service delivery, providing continuity of care, and building a strong foundation for the sector.
Key recommendations
Specifically, we are asking the government to prioritize the following three areas for sector stability:
- Begin to close the wage gap through a three-year targeted funding commitment that delivers on the community child and youth mental health portion of the For Us. For You recommendations from Ontario’s community health sector.
- Develop a health human resources strategy for the sector because we know that while wages are a significant part of the challenge, additional policy opportunities and strategies that attract professionals into the sector and prevent turnover into other service systems must also be considered.
- Ensure the health human resources challenges and wage gaps are addressed across the system of care for children and youth. For example, MCCSS-funded infant and young parent programs and youth justice programs must be included in both the new funding to close the wage gap and the workforce planning strategy. In addition, many child and youth mental health agencies are multi-service providers, so impacts on funding and wages for one program area have impacts across the entire organization.
SUSTAIN
The child and youth mental health sector is eager to partner with the government to streamline processes and strengthen sector capacity to ensure data is consistently available, collected, and evaluated across child and youth mental health.
Key recommendations
We want to partner with the government to:
- Develop and implement a data strategy to enable child and youth mental health to advance system quality improvement, including standardized data collection and evaluation. The collection and utilization of data to support service delivery and system improvement is an important part of building system approaches in the child and youth mental health sector, and it enables the sector to better understand the impact of new investments and more effectively plan for the future.
- Collect identity-based data in recognition of the important role that this data can play in helping agencies measure existing inequities and disparities to inform service delivery and evaluate progress. By identifying and prioritizing data collection, the opportunity is created to improve mental health outcomes for racialized and equity-deserving infants, children, youth, and families.
- Develop a strategy to look at no-cost and low-cost solutions to improve planning and service delivery and reduce added administrative and operational pressures, such as moving towards three-year funding agreements and streamlining reporting and policies across Ministries and Ontario Health, so that more funding can go towards enhancing service delivery, improving outcomes, and reducing wait times.
SYSTEM BUILD
Addressing service gaps and ensuring timely access to high-quality mental health services for children and youth across Ontario is crucial for system improvement. Targeted investments are needed to address gaps in care.
Key recommendations
Meaningful and collaborative engagement with those with lived experience in the system provides a significant opportunity to support children, youth, and families, while also building expertise for system design.
- Support child and youth mental health to implement a Health Equity Strategy for the sector. Health inequities across the province mean that some children and youth are not able to access culturally-responsive services or services altogether due to service gaps. Prioritizing a strong equity focus acknowledges the significant influence of the social determinants of health on mental health outcomes and includes a commitment to ensuring accessible and quality services for populations such as Black, Indigenous, 2SLGBTQ+, Francophone, and immigrant communities and other equity-deserving groups.
- Close gaps by targeting investments and strategies that build the system for populations and communities across Ontario. Across several populations of children and youth and intersections with mental health, there is a need to advance approaches to fill service gaps and expand front line services, while also connecting with initiatives that are building more coordinated, integrated, and planned approaches in the system. By focusing on closing gaps through a system-building lens, we can advance provincial work to enable local service system improvement. For example, recent investments in children’s health and pediatric care have enabled system building and addressing gaps in care, particularly for children and youth with intensive needs through the Ontario Intensive Treatment Pathway (OITP). With an added investment and strategy, the sector would be able to advance system design and improvement.
- Collaborate with youth and families with lived experience to ensure that new initiatives and system building are centered on the needs of infants, children, youth, and families. To help build system capacity to support youth and family-led change, CMHO is requesting new funding of $676,000 a year to expand The New Mentality (TNM) and Parent’s for Children’s Mental Health (PCMH) programs that support youth and family engagement, as well as deliver family peer support through networks and chapters all across Ontario.
Building on Our Success
The community child and youth mental health sector is eager to partner with government and across children and health service systems to advance a system that places the integrated needs of children and families at the centre. We recognize that it is not just about more money to do more of the same—we need new ways of working, to be creative about how we leverage resources, and to focus most importantly on putting the needs of infants, children, youth, and families at the centre.
Child and youth mental health agencies have shown leadership and creativity, even in the face of significant funding constraints. With new investments and policy supports from the province, there are strong foundations to build on in community child and youth mental health that are important examples of system building and improvement.
Every window where we can intervene early is a chance to change a child’s entire life for the better. Children are our future, and investments in their mental health lead to savings and better outcomes both today and for decades to come. Our kids and families can’t wait.
